“ I’m Worried About my Wound…” — Stress, Anxiety, Pain and Wound Healing

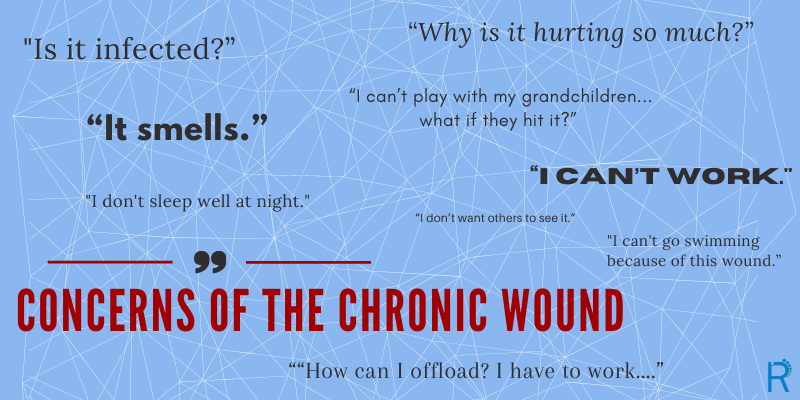
These are some of the concerns persons with chronic wounds have shared. Wounds, especially when they are painful, can cause anxiety and stress.
Can anxiety, stress, and pain slow wound healing, and if so, what can practitioners and persons with wounds do?
Wounds that do not heal in a timely fashion cause stress. Persons with chronic wounds often express concern as to why the wound is taking so long to heal and even wonder if it will ever heal. This affects their quality of life and this stress can contribute to increased pain in the wound. Pain with dressing changes or going to bed when leg elevation causes increased hypoxia, can lead one to anticipate pain, triggering a stress response.” As an unpleasant physical and emotional experience, pain induces stress leading to a cascade of physiological events that stall wound healing” (Woo, 2012).
“A stress response can result in the overproduction of cortisol and catecholamines resulting in a significant impact on wound healing due to alteration in the immune system and tissue hypoxia” (Kiecolt-Glaser, Marucha, Malarkey, Mercado, Glaser, 1995).
Chronic tissue hypoxia will lead to slowed wound healing and may increase pain in sensate wounds, and potentially increase stress and anxiety.
“Wound pain can lead to hypoxia which impairs wound healing and increases infection rates. As tissue oxygen decreases, there is a decrease in the production of leucocytes which provides opportunity for bacteria to colonise the wound thus leading to infection” (Frescos, 2011).
Wounds not only damage tissue, but can also harm emotional and psychological wellbeing and quality of life. Wound care practitioners often recommend behavioral changes that will help with wound healing – smoking cessation, weight loss, lowering of A1C, but consideration must also be given to the stress and anxiety induced by these recommendations. When stress/ anxiety and pain increase, there is a decrease in oxygen levels in the tissue surrounding the wound. “It is important to consider the interconnection between stress, anxiety, pain, and wound healing and to offer education and management strategies through supportive therapeutic communication" (Woo, 2012).
Suggestions for reducing the harmful effects of stress, anxiety, and pain on wound healing:
- Discuss the effects of stress, anxiety and pain on wound healing with your patient to engage them in self-awareness and to empowerment them in self-care
- Watch for signs of increased pain and stress as this may be an indicator of physical changes in the wound, such as infection, ischemia, edema, nerve damage, increased pressure on tissue
- Increase knowledge about wound care products that can reduce symptoms of pain, such as non/ adhering dressings, gentle interface surface, antimicrobial (if bio-burden a problem), and topical continuous diffusion of oxygen. (Bowen, Ingersol &Carlson, 2018)
- Exercise (Mayo Clinic Staff, nd)
- Nutrition (Naidoo U, nd)
- Consider referral to specialist in management in stress/anxiety and pain
- Consider pharmacological measures for stress/anxiety and pain
- Meditation, music therapy, support/ social groups, journalling (Meesters et al., 2018)
Exploring the role of hypoxia and wound healing further, Sen (2009) notes that a common factor in the aetiology of most chronic wound cases is extreme hypoxia. Observing someone with lower limb ischemia, one is made acutely aware of the intensity of pain that ischemia and hypoxia can cause. As many chronic wounds are at risk of hypoxia because of the aetiology, pain and stress are likely to be intwined. Stress/anxiety may increase pain, pain may increase stress/anxiety, and compounded in a chronic wound, may result in decreased oxygenation to the wound. By providing oxygen directly to the wound through continuous diffusion of moist 100% oxygen (such as the OxyGeni System), tissue hypoxia can be reduced, and potentially pain and stress/ anxiety reduced and wound healing improved.
Clinicians caring for persons with chronic wounds, need to consider all factors contributing to wound healing or not healing, and offer education, support, and treatments that meet the needs of the person and their wound in a holistic manner.
This blog post was written by Kathryn Mutch, BN, RN, NSWOC, WOCC(C)
Nurse consultant for EO2.
What is BN, RN, NSWOC, WOCC(C)? A nurse specialized in wound, ostomy, continence, and Canadian Nurses Association certification

