Lower Extremity Amputations: Why, What Kind, & Life After

Every year, surgeons perform a lower-limb amputation due specifically to diabetes on approximately 73,000 patients in the US alone. Annually there are over 1 million limb amputations worldwide. Most of these amputations are performed for the treatment of non-healing diabetic foot ulcers that resulted from PAD (Peripheral Arterial Disease). These non-healing foot ulcers are caused by high blood glucose levels, which accelerate the direct damage to the nerves and blood vessels in the body, specifically the limbs. When left untreated, PAD can have serious complications, resulting in amputation, in its most severe form.
Leg or foot amputation due to diabetes can have significant physical and emotional consequences, not only for the person with the amputation, but to his or her loved ones as well. The most unfortunate part is, some of these amputations could have been avoided if only the patient had gotten proper medical care early on.
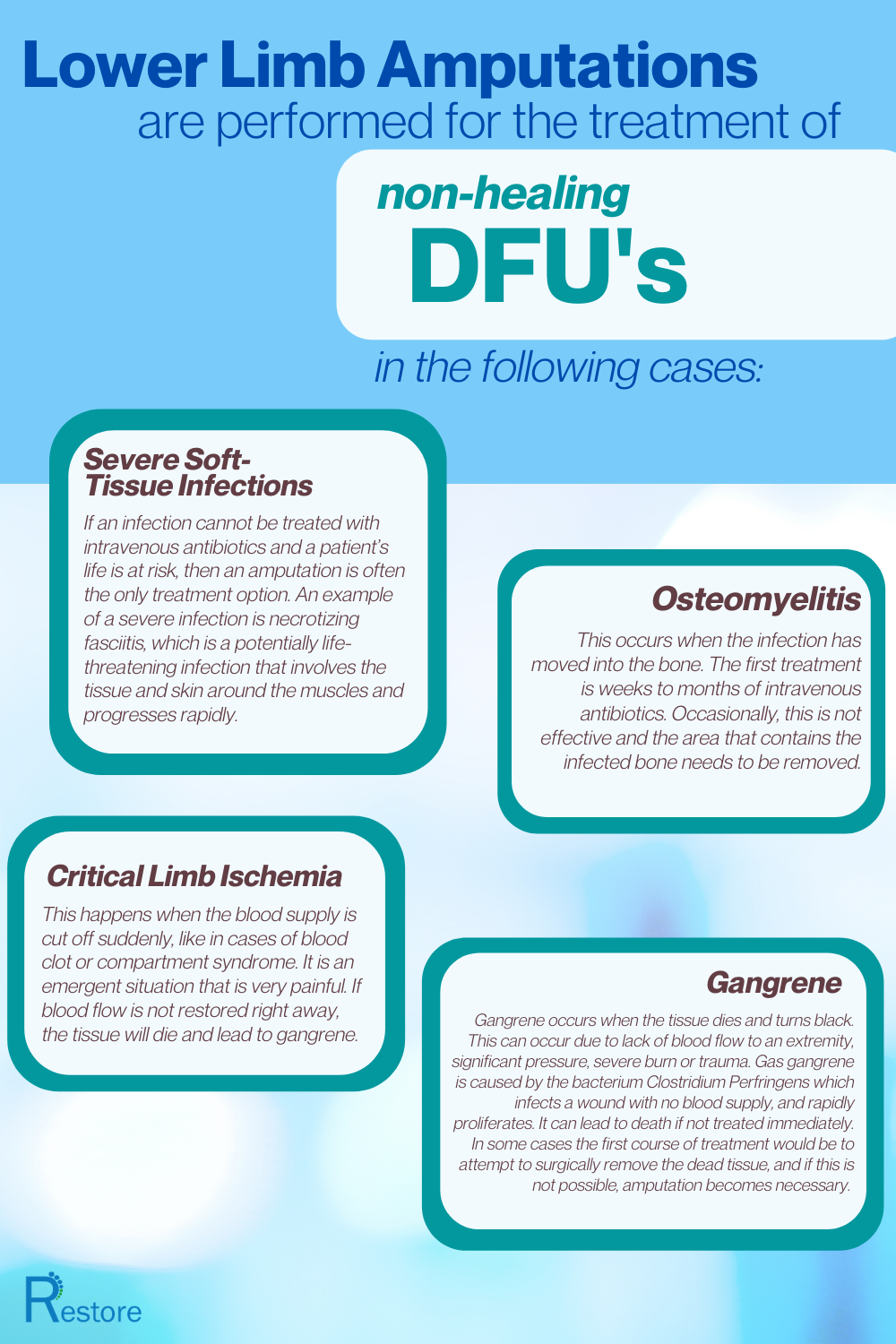
Severe Soft-Tissue Infections:
If an infection cannot be treated with intravenous antibiotics and a patient’s life is at risk, then an amputation is often the only treatment option. An example of a severe infection is necrotizing fasciitis, which is a potentially life-threatening infection that involves the tissue and skin around the muscles and progresses rapidly.
Osteomyelitis:
This occurs when the infection has moved into the bone. The first treatment is weeks to months of intravenous antibiotics. Occasionally, this is not effective and the area that contains the infected bone needs to be removed.
Critical Limb Ischemia:
This happens when the blood supply is cut off suddenly, like in cases of blood clot or compartment syndrome. It is an emergent situation that is very painful. If blood flow is not restored right away, the tissue will die and lead to gangrene.
Gangrene:
Gangrene occurs when the tissue dies and turns black. This can occur due to lack of blood flow to an extremity, significant pressure, severe burn or trauma. Gas gangrene is caused by the bacterium Clostridium Perfringens which infects a wound with no blood supply, and rapidly proliferates. It can lead to death if not treated immediately. In some cases the first course of treatment would be to attempt to surgically remove the dead tissue, and if this is not possible, amputation becomes necessary.
The goal of amputation is successful healing while preserving as much function as possible and creating a residual limb that will work best with or without a prosthesis. Other issues that affect decisions about the type and extent of surgery include the patient’s overall health and his or her ability to withstand anesthesia, the level at which there is adequate blood flow, the potential successful rehabilitation, and the desired activity level afterward.
An understanding of skeletal and vascular anatomy of the leg, foot, and toes is key in amputations.
Syme Amputation:
Disarticulation of the foot with removal of both malleoli, followed by forward rotation of the heel pad over the end of the residual tibia. This technique provides an end-bearing stump that allows ambulation over short distances. The residual limb ends at the distal base of the tibia. A complication of the Syme amputation is migration of the heel pad, which is not firmly fixed to the tibia.
Terminal Syme Amputation:
Amputation of part of the distal phalanx, which is performed via an elliptical incision and involves resection of the toenail, nail bed, and approximately half of the distal phalanx. The wound is closed by placing the skin flap over the stump and suturing the skin.
Boyd Amputation:
Similar to Syme amputation but provides a broad weight-bearing surface of the heel by creating an arthrodesis between the distal tibia and the calcaneus. This provides more length and better preserves the weight-bearing function of the heel pad than the Syme. The Boyd amputation preserves the calcaneus, and the calcaneus is fused to the tibia. This relieves the problem of migration of the heel pad because the heel pad remains firmly attached to the calcaneus. Both malleoli are also preserved.
Chopart Amputation:
Midtarsal amputation of the foot between the calcaneus, cuboid bones, talus, and navicular bones.
Lisfranc Amputation:
Amputation of the foot between the metatarsus and tarsus (tarsometatarsal joint), which is located between the base of the first through fifth metatarsal bones and their connection with the medial, intermediate, and lateral cuneiforms and the cuboid bone in the foot.
Transmetatarsal Amputation:
Amputation of all toes at the level of the metatarsals (neck region)
BKA (Below Knee Amputation):
Amputation at below knee level
AKA (Above Knee Amputation):
Amputation at above knee level
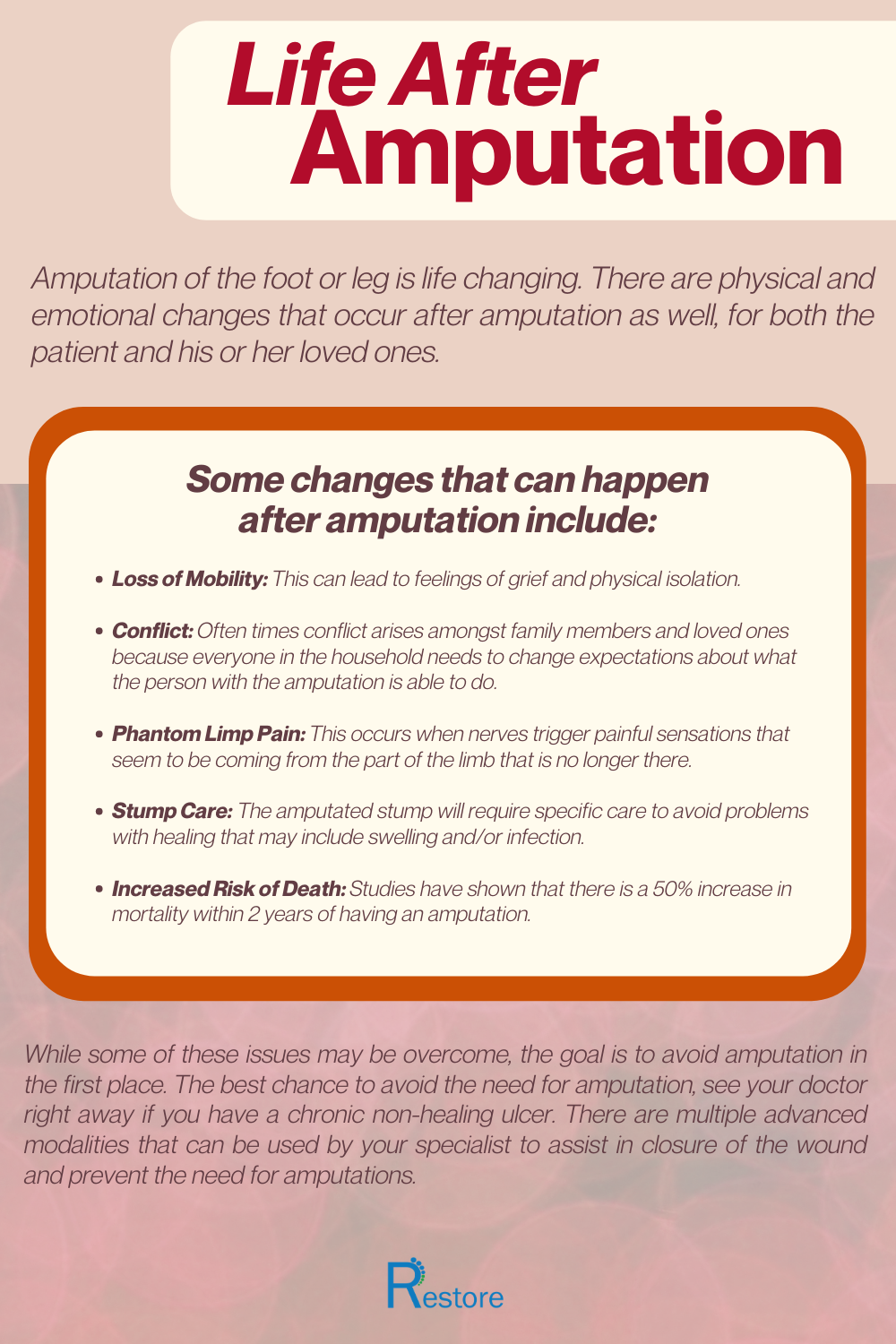
Life After Amputation
Amputation of the foot or leg is life changing. There are physical and emotional changes that occur after amputation as well, for both the patient and his or her loved ones.

- Loss of Mobility – This can lead to feelings of grief and physical isolation.
- Conflict – Often times conflict arises amongst family members and loved ones because everyone in the household needs to change expectations about what the person with the amputation is able to do.
- Phantom Limp Pain – This occurs when nerves trigger painful sensations that seem to be coming from the part of the limb that is no longer there.
- Stump Care- The amputated stump will require specific care to avoid problems with healing that may include swelling and/or infection.
- Increased Risk of Death – Studies have shown that there is a 50% increase in mortality within 2 years of having an amputation.
While some of these issues may be overcome, the goal is to avoid amputation in the first place. The best chance to avoid the need for amputation, see your doctor right away if you have a chronic non-healing ulcer. There are multiple advanced modalities that can be used by your specialist to assist in closure of the wound and prevent the need for amputations.

This blog post was written by Babak Nouri , DPM and Wound Care Specialist for EO2 Concepts
in NYC.
What is DPM? A doctor of podiatric medicine. A medical professional devoted to the treatment of disorders of the foot, ankle and lower
extremity.
Shareable Graphics: